Sleep FAQs
Stephen Deal • May 23, 2019

Below are some frequently asked questions that Dr. Deal receives all the time. Sleep is such a vague process and sometimes it is hard to understand not only the terminology but also what is happening during our sleep issues. I hope that this information can answer some of your questions about sleep. If you are having trouble sleeping, are intolerant to your current CPAP device, or just want to ask more questions about what we can do to help, please give us a call at (501)500-5105 to set up your free consult appointment.
- My doctor says I’m at risk for sleep apnea, what does that mean?
Sleep apnea is a common disorder in which you have one or more pauses in breathing or shallow breaths while sleeping. The most common type of sleep apnea is obstructive sleep apnea, a condition in which the airway collapses or becomes blocked during sleep. When your doctor tells you that you are at risk for this condition, they are saying that your airway is already undersized and that when you lie down in certain positions, the soft tissue surrounding the airway is likely to collapse and obstruct the airflow causing these pauses in breathing.
- How does sleep apnea affect me?
The consequences of these sleep disorders if left untreated include cardiovascular disease, heart failure, stroke, high blood pressure, diabetes, and premature death. Studies have shown that OSA is linked to all of those conditions, but more immediately, obstructive sleep apnea affects your rest and the quality of sleep you get. The interruptions in breathing do not allow the body to enter the deep sleep cycles that are most useful to us. Therefore, even though people think they are sleeping they can be exhausted during the day because they are not getting “restful” sleep at night.
- What causes snoring?
Snoring, the sounds made when sleeping, is a separate sleep disorder but one that is often associated with sleep apnea. Snoring is caused by the sound of the soft tissue surrounding the airways (tonsils, tongue, soft palate, adenoids, soft tissue lining of the pharynx, etc.) flapping as air travels through the space. In other words, when a breath passes through the pharynx (throat) to the lungs it is flapping the soft tissue against the walls of the airway and that is the sound that we know as snoring. Obviously if the airway is narrowed or collapsed as it is in patients with OSA, there is more flappy tissue and the snoring sounds louder as the person breathes during sleep.
- If I don’t snore, can I still have sleep apnea (OSA)?
○Yes! There are cases where the reason the airway is narrowed is not due to flappy soft tissue obstructing the path, but rather due to some anatomical or systemic issues (asthma, respiratory conditions) that leave the airway narrow but solid.
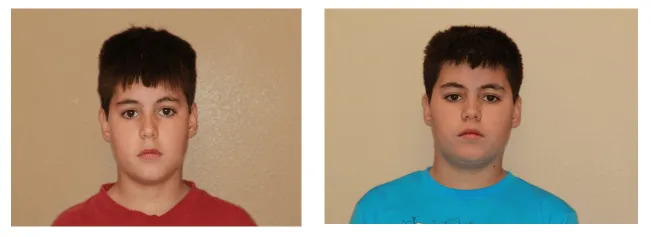
- Can Children have sleep apnea (OSA)?
○Absolutely. Pediatric sleep apnea is a very common, but often undiagnosed finding. Enlarged tonsils and adenoids can often be the obstruction in the airway causing childhood sleep issues, however, it can also be due to the posterior position of the children’s jaws that encroach on the airway. 80% of the population have an undersized top jaw which leads to a cascade of effects on the facial structure and airway volume. Pediatric sleep apnea can be a scary thing. Here is a video showing how a child with sleep apnea sleeps. Viewer discretion is advised!! https://www.youtube.com/watch?v=3GON9iqIH9A&t=56s
- What are some signs that my child has sleep apnea?
○There are many signs that your child is suffering from sleep apnea or sleep disordered breathing. If you are in a separate room or sleep far from your child, it can be hard to notice if they are having the same issues as the child in the link above. Luckily there are some other signs that can help you notice. First off if you hear them grinding their teeth at night (can be very loud sometimes) or notice their baby teeth are getting really worn down, they are likely to have some pauses in breathing during their sleep. The grinding is caused by the lower teeth sliding against the upper teeth as the lower jaw is forcing itself forward and out of the airway so the child can breathe. Some other signs are dark circles under the eyes (poor sleep), behavioral issues (linked to ADHD), bedwetting issues, or ear problems with or without infections. If your child is experiencing any of these issues and a solution can’t be found, the quality of their sleep should be examined, and pediatric sleep apnea should be considered as a potential cause.